Degenerative disc disease (osteochondrosis) in the chest is a relatively rare condition compared to other thorns. This is because the chest stabilizes the thoracic vertebrae, limiting movement and injuries from constant bending and stretching, as happens in the rest of the spine. If osteochondrosis develops in the thoracic spine, then most often its development is associated with trauma.

Degeneration, destruction and inflammation in the area of the disc can cause a number of symptoms, depending on the severity of the problem. Disc pathology can lead to symptoms such as reduced range of motion in the back, back pain that may radiate to the intercostal space, tingling, numbness, muscle spasm, or certain combinations of these symptoms. The most common manifestations of osteochondrosis in the chest area occur at the level of T8-T12. As a rule, the manifestations of osteochondrosis in the thoracic region are: protrusion, disc extrusion, herniated disc with sequestration, spondylolisthesis.
Treatment of thoracic osteochondrosis is most often conservative, but in the presence of complications such as spinal cord compression, surgical treatment is possible.
Osteochondrosis (degenerative disc disease) is not actually a disease, but a term used to describe progressive changes in the discs associated with progressive wear and tear and the development of symptoms secondary to disc degeneration. Disc degeneration is a normal involutionary process, but in certain situations the degeneration process can be accelerated, for example as a result of trauma, overuse, and musculoskeletal imbalances such as scoliosis. Disc degeneration is not a problem in itself, but the conditions associated with it can lead to the development of advanced symptoms.
Stages of disc degeneration
The progression of disc degeneration can be classified into the following stages:
Dysfunction
- Ruptures in the area of annular fibrosis are possible, with irritation of the facet joints at the appropriate level of the spine.
- Loss of joint mobility, local back pain, muscle spasm and limitations in trunk mobility, especially elongation.
Instability
- Disc fluid loss with dehydration and disc height reduction. Weakness of the facet joints and capsules may develop, leading to instability.
- The patient will experience shooting pain, straightening of the spine and a sharp decrease in the range of motion in the trunk.
Re-stabilization
- The human body reacts to instability by forming additional bone formations in the form of osteophytes, which to some extent help to stabilize the spine. But excessive bone formation can lead to spinal stenosis.
- Back pain usually decreases, but remains less intense. Some people may develop symptoms similar to stenosis.
The reasons
- Involuntary changes in the body are the most common cause of disc degeneration. As the body ages, the discs gradually lose their fluid part and become dehydrated. The discs begin to narrow and lose their height, impairing their ability to absorb shock and stress.
- The outer annular fibrous structures of the disc may begin to crack and tear, weakening the walls of the disc.
- People who smoke, become obese, and engage in strenuous activities are more likely to develop disc degeneration.
- Injury to the spine or disc from a fall or impact can trigger the degeneration process.
- Disc herniation can initiate the development of disc degeneration.
- Unlike muscles, discs have a minimal blood supply, so they do not have reparative capacity.
Symptoms
The symptoms associated with osteochondrosis of the chest will depend on the location and structures involved in this process. Disc degeneration in the thoracic spine can affect the back, the area under the shoulder blade, or along the ribs.
- Many patients with degenerative disc disease of the chest may have no symptoms.
- Chronic chest pain with / without irradiation of the ribs.
- Sensory changes such as tingling, numbness or paraesthesia in cases where there is compression of the nerves.
- Muscle spasm and changes in posture in the chest.
- Loss of range of motion, with reduced ability to move the boot, especially when turning or bending sideways.
- Sitting for long periods of time can cause back pain and arm pain.
- Difficulty lifting weights and lifting arms above the head.
- In the later stages, spinal stenosis may develop, leading to weakness in the lower extremities and loss of coordination. In these cases, surgery will be required.
Diagnosis
In addition to conducting an in-depth examination, the doctor may order the following tests to verify the diagnosis:
- X-rays,helps determine if there is joint degeneration, fractures, bone malformations, arthritis, tumors or infection.
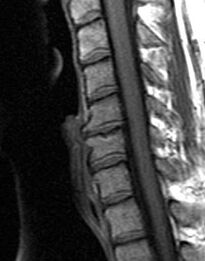
- NMRto determine morphological changes in soft tissues, including visualization of discs, spinal cord, and nerve roots.
- CT scana scan that can provide cross-sectional images of vertebral structures.
- EMG,this diagnostic method is used to determine nerve damage and the level of damage.
- Myelogramas a rule, this method of examination is necessary to clarify the morphological changes in the degree of impact on the roots and spinal cord and to plan surgical intervention.
Treatment
The treatment of osteochondrosis of the chest will depend on the severity of the condition.
Treatment of acute pain syndrome:
- Rest: Avoid activities that cause pain (bending, lifting, twisting, twisting or stretching backwards).
- Medicines to reduce inflammation (anti-inflammatory drugs and painkillers).
- Ice in acute cases can relieve spasm, relieve pain.
- Local heat exposure can help relieve pain and muscle tension.
- Light gymnastic exercises to eliminate biomechanical disorders associated with osteochondrosis and improve joint mobility, normal configuration of the spine, posture and range of motion.
- It may be necessary to use a brace to relieve stress on the facet joints and chest muscles.
- Corticosteroids are used to reduce inflammation in moderate to severe cases.
- Epidural injections directly into the area of the damaged disc.
In mild cases, the use of local colds and medications may be enough to relieve the pain. After relieving the pain, exercises (physical therapy) and exercises to stretch and strengthen the back muscles are recommended. The return to normal activity should be gradual to prevent recurrence of symptoms.
The main conservative methods for the treatment of osteochondrosis of the chest
Medication treatment
The task of using drugs in the treatment of osteochondrosis of the chest, especially in acute pain syndrome, is to reduce pain, inflammation and muscle spasm.
- OTC medications for mild to moderate pain.
- Narcotic analgesics for intense pain that cannot be controlled by other treatments.
- Muscle relaxants to reduce acute muscle spasm.
- Prescription analgesics.
- Injections such as facet joints, obstructions or epidural injections. These may include injecting corticosteroids into specific areas to reduce local inflammation.
- Manual therapies, including soft tissue massage, stretching and joint mobilization, performed by a specialist, improve the geometry, mobility and range of motion in the thoracic spine. The use of mobilization techniques also helps to modulate pain.
- Exercise therapy (therapeutic exercises), including exercises to stretch and strengthen the muscles, to restore range of motion and strengthen the muscles of the back and abdomen, support, stabilize and reduce stress on the discs and back. An exercise program, especially exercises with weights or weights, should be started after the pain, muscle spasm and inflammation have subsided. Improperly selected exercise program can worsen symptoms. Therefore, the selection of exercises should be done with an exercise therapy doctor.
- Neuromuscular retraining to improve posture, restore stability, teach the patient the correct biomechanics of movement to protect damaged discs and spine.
- Physical therapy, including the use of ultrasound, electrical stimulation and a cold laser, helps reduce pain and inflammation of the spinal structures.
- Home exercise programs, including exercises to strengthen muscles, stretch and stabilize, and make lifestyle changes to reduce stress on the spine.
- Acupuncture. This method of treatment can be used in the presence of sensory disturbances or to restore conduction and reduce pain.
Surgical treatment
Most hernias located in the thoracic spine of the thoracic disc can be successfully treated without surgery. However, when conservative treatment of thoracic osteochondrosis is ineffective, surgery may be recommended, especially if the patient has any of the following symptoms:
- Increased radicular pain.
- Increased pain and nerve damage.
- Development or increase of muscle weakness.
- Increased tingling or paresthesia.
- Loss of control over bowel and bladder function.
The most common operation involving disc degeneration is discectomy, in which the disc is removed by incision. However, there are several surgical procedures that can be recommended in cases of osteochondrosis and disc degeneration. The choice of surgical method depends on the cause of the symptoms. Basic surgical techniques - include foraminotomy, laminotomy, spinal laminectomy, spinal decompression and spinal fusion.
Forecast
Most of the problems associated with osteochondrosis of the thoracic spine can be solved without surgery and people return to normal work. Osteochondrosis in the thoracic spine due to anatomical rigidity develops less than in other parts. The duration of treatment, as a rule, does not exceed 4-12 weeks and depends on the severity of symptoms. Patients should continue with the program of stretching, strengthening and stabilization. A good long-term prognosis requires the use of proper movement and body mechanics and an awareness of the importance of maintaining the health of the spine.































